Deep Brain Stimulation (DBS)
Overview
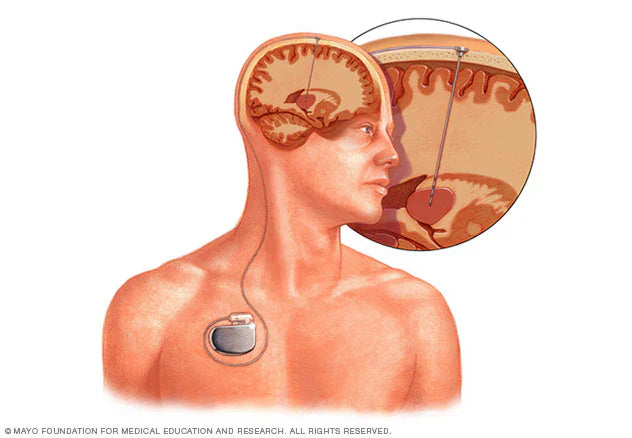
Deep brain stimulation (DBS) involves implanting electrodes into specific areas of the brain. These electrodes deliver electrical pulses that affect brain activity to treat certain conditions. The pulses can also affect the brain's cells and neurotransmitters that cause the condition.
The level of stimulation in DBS is controlled by a pacemaker-like device placed under the skin in the upper chest. A wire runs under the skin connecting this device to electrodes in the brain.
Deep brain stimulation is commonly used to treat a number of conditions, such as:
- Parkinson's disease.
- Essential tremor.
- Diseases that cause dystonia, such as Meige syndrome.
- Epilepsy.
- Tourette syndrome.
- Obsessive-Compulsive Disorder (OCD).
Deep brain stimulation is also being studied as a potential treatment for:
- Chorea, like Huntington's disease.
- Chronic pain.
- Cluster headache.
- Dementia.
- Depression.
- Addiction.
- Obesity.
Why deep brain stimulation?
Deep brain stimulation is a proven treatment for movement disorders, including essential tremor, Parkinson's disease, and dystonia. It is also used for some psychiatric disorders, such as OCD. The U.S. Food and Drug Administration (FDA) has also approved DBS for reducing seizures in difficult-to-treat epilepsy.
DBS is usually prescribed for people whose symptoms cannot be controlled with medication.
Risk
DBS is generally considered to be low risk. However, any surgery carries a risk of complications, and brain stimulation can cause side effects.
Risks of surgery
DBS (deep brain stimulation) involves drilling small holes in the skull to place electrodes into brain tissue, and surgically implanting a pacemaker-like device under the skin in the chest. This device contains the battery needed for deep brain stimulation. Surgical complications may include:
- Lead misplacement.
- Cerebral hemorrhage.
- Stroke.
- Infection.
- Shortness of breath.
- Nausea.
- Cardiovascular problems.
- Convulsions.
Side effects after surgery
- Convulsion.
- Infection.
- Headache.
- Confusion, difficulty concentrating.
- Stroke.
- Hardware complications, such as worn electrode wires.
- Temporary pain and swelling at the implant site.
A few weeks after surgery, the device will be activated and your doctor will begin adjusting the settings accordingly. Some settings may cause side effects, but these usually improve after adjustment.
There have been rare reports that DBS may affect the movements required for swimming. Patients should consult their doctor before swimming and follow water safety guidelines.
Side effects of stimulation
- Numbness or tingling sensation.
- Facial or arm muscle tension.
- Hard to say.
- Loss of balance.
- Dizzy.
- Changes in vision (such as double vision).
- Mood changes: irritability, mania, depression.
How to prepare
First, consider the benefits and risks.
DBS is a complex procedure with potential risks. If you qualify, you should discuss the benefits and risks with your doctor.
Then, prepare for surgery
Patients will need to undergo medical tests to ensure safety. Brain imaging techniques such as MRI are often prescribed to determine the exact location of electrode implantation.
What can you expect?
In surgery
In general, DBS surgery is performed as follows:
Brain surgery
During brain surgery, the medical team will attach a special stereotactic head frame to your head. This will hold your head still during the procedure. Neuroimaging techniques such as MRI or CT scans will then be used to map your brain. These images will help determine the exact location of the electrodes.
Usually, the electrodes are placed when the patient is awake and fully conscious. This allows the doctor to immediately check the effectiveness of the stimulation. If you are awake, you will be given a local anesthetic to numb your scalp before the surgery. The brain does not have pain receptors, so no anesthesia is needed in the brain. In some cases, the surgery may be performed under general anesthesia.
The surgeon will implant a thin wire (lead) with several small electrodes on the end into the targeted area of the brain. Some patients have electrodes placed on both sides of the brain (a total of two electrodes). One lead will run under the skin, connecting to a device called a pulse generator, which is implanted under the skin near the collarbone.
During surgery, your neurologist and neurosurgeon will work together to monitor your brain activity to make sure the electrodes are placed correctly.
Chest wall surgery
During the second stage of the surgery, the surgeon will implant a pulse generator under the skin of the chest, near the collarbone. This device contains a battery that powers the system.
During this procedure, the patient is given general anesthesia. Leads from electrodes in the brain are placed under the skin and guided down to connect to a battery-powered pulse generator.
A few weeks after surgery, the pulse generator will be programmed during a follow-up visit with your doctor. Once programmed, the device will send continuous electrical pulses to your brain. You can control the device with a special remote control, which can be turned on and off as needed.
After surgery
A few weeks after surgery, the pulse generator in your chest will be activated, usually at your doctor's office. The pulse generator can be programmed from outside your body using a special control device.
The level of stimulation will be individualized to suit your condition. It can take 4 to 6 months to find the optimal setting.
Stimulation may be continuous 24 hours a day, or you may be instructed to turn the device off at night and on again in the morning, depending on your condition. You can turn the device on and off using a remote control that you carry with you. In some cases, the device can be programmed to allow you to make minor adjustments yourself at home.
The pulse generator's battery life varies depending on the frequency of use and the settings. When the battery is low, the surgeon replaces the pulse generator during an outpatient procedure.
Result
DBS does not cure the condition, but it can significantly reduce symptoms. Symptoms may improve to the point of making a noticeable difference, but they often do not go away completely. In some conditions, you may still need to take a combination of medications.
The effectiveness of DBS varies from person to person and depends on many factors. Patients should discuss this with their doctor before surgery to determine the level of improvement they can expect.
Source: mayoclinic.org
-------------------------------------------------------------------------------------------
👉 Contact SunCare for medical support and advice as well as professional private jet transportation services 🇸🇬 SUNCARE PTE. LTD SINGAPORE
🏠 Add: 10 Anson Road, #10-11 International Plaza, Singapore 079903
☎️ Hotline: +65 96727717 (Dr. Lien Minh - Director) Zalo, Viber
📨 Email: suncarehealth@gmail.com






